When a new resident arrived at Brantford’s Hardy Terrace Long-Term Care facility in the fall of 2023, RN Dalal Isbiteh and her colleagues knew exactly what to do to ensure he was admitted properly. Using RNAO Clinical Pathways, an evidence-based software derived from best practice guidelines (BPG), the team completed a comprehensive assessment to document his daily routine and health.
“(You go) from no information to almost everything you need to know about the resident within a short period of time,” Isbiteh says. The information they collected, which draws on recommendations in RNAO’s Delirium, Dementia and Depression in Older Adults: Assessment and Care BPG, is then stored in the home’s secure electronic medical records system.
By the evening, the resident started to act differently. He was confused, moving around a lot and not answering questions. The nurses who came for the evening shift went back to the detailed admission information that revealed “…he had a recurrent UTI [urinary tract infection] and he gets delirium with his UTIs,” Isbiteh explains. He was sent to the hospital and successfully treated for delirium over a number of days.
Isbiteh looks back on the experience with appreciation for the home’s use of the RNAO Clinical Pathways and its ongoing partnership with the association as a Best Practice Spotlight Organization® (BPSO®). It has had a tremendous impact on delirium care and outcomes, she says.
Between 2022 and 2024, the percentage of residents assessed for delirium risk factors at the initiation of care increased from zero to 100 per cent. The percentage of at-risk residents with delirium prevention plans also rose, from just under one per cent to 100 per cent. The home has consistently maintained low delirium incidence rates among its residents since 2022. There was some minor fluctuation in these numbers, but that was largely attributed to the COVID-19 pandemic.
RNAO Clinical Pathways allow long-term care homes across the province to measure the impact of the BPGs they are implementing.
“We provide them with evidence-based performance indicators,” explains Rita Wilson, senior program manager. “Once they implement the clinical pathways, their data is sent to RNAO’s Nursing Quality Indicators for Reporting and Evaluation® (NQuIRE®) data system for processing, and reports are generated for the homes to use to support their own quality improvement initiatives.”
With the data collected, RNAO partners with organizations to produce an Evidence Booster, a two-page infographic that showcases the results. Dr. Shanoja Naik, director of the RNAO Research Unit, says access to data in daily practice is critical to understanding gaps in care, measuring improvement and demonstrating impact. “We began publishing Evidence Boosters almost a decade ago and these are extraordinary tools to show – with hard data – the impact of BPGs. Any organization implementing BPGs should strive for publication of their data to share their journey and inspire others.”
“BPGs are making a marked difference in long-term care,” says Janet Chee, associate director of guideline implementation and knowledge transfer, and the former associate director of the long-term care BPG program at RNAO (now being led by Dr. Julia Fineczko). “We see results for residents … improvement in quality of life for residents. Everything built around these RNAO Clinical Pathways has the resident in mind.”
The impact of BPGs is seen also in all other sectors.
At CBI Home Health – a BPSO and large home care and specialized community service provider in Canada – Kathy Mazza, manager of clinical excellence, says BPGs have helped with wound care for clients.
“It’s one of the best guidelines that we’ve implemented to be honest. It’s made a big difference,” she says, referencing the data shared in an Evidence Booster in October 2024.
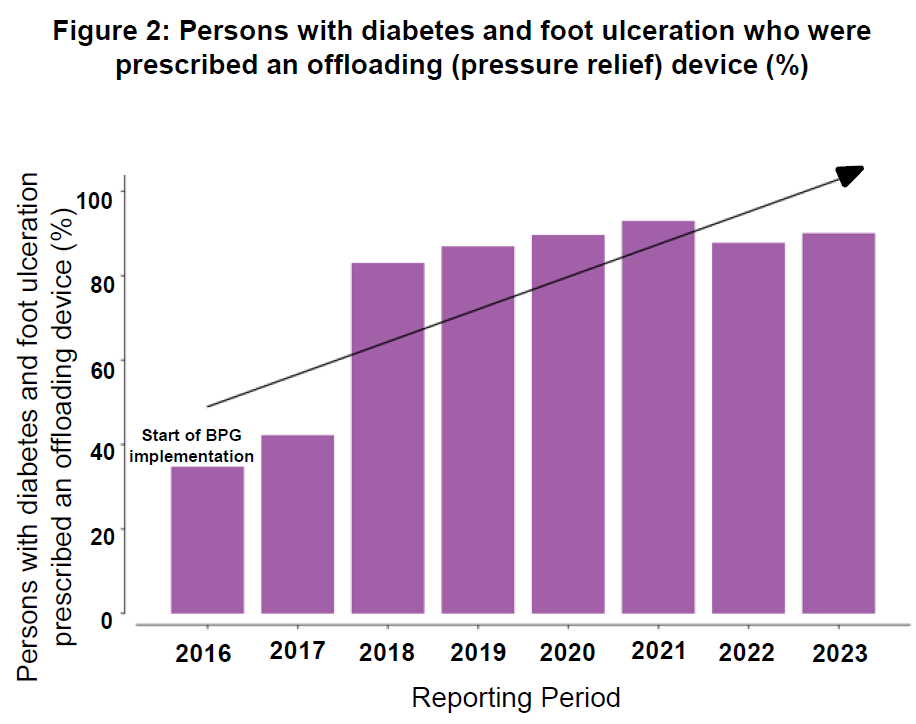
Between 2016 and 2023, CBI Home Health implemented Assessment and Management of Foot Ulcers for People with Diabetes (2013) (in October 2024 this BPG was replaced with Diabetic foot ulcers: Prevention, assessment and management). As a result, they are now seeing more than 90 per cent of patients with diabetes and foot ulceration consistently assessed for problems with lower extremities. They have also seen a 55 per cent increase in the percentage of clients prescribed an offloading (pressure relief) device, helping with disease management, foot care and ulcer care.
Measuring impact without numbers
This hard data collected through NQuIRE is vital to determine the impact of BPGs. Yet, it’s not the only way to measure progress and improvement.
At the Sarnia-Lambton Ontario Health Team (OHT), processes are becoming more efficient and standardized across the health-care continuum thanks to BPGs. Instead of having patients repeat information they’ve already provided to one organization, everything is uploaded into a shared system, so assessments take less time.
“We have a number of community support agencies that are uploading and sharing their assessments across the board,” says Nadine Neve, executive lead.
Guideline implementation, which includes work on the Person- and Family-Centred Care BPG – a mandatory BPG for all BPSOs – has also enhanced collaboration and communication between OHT partners. “We’re able to reach a number of partners pretty easily and share the information and those best practices with smaller organizations that may or may not have access to them,” says Neve. “Through the development of learning modules based on the BPGs, OHT partners are collaborating, and patients are benefitting.”
Jane Mathews, chief nursing executive and vice president of clinical support services at Bluewater Health, a BPSO and Sarnia-Lambton OHT partner, says they’re “seeing some really great responses coming back from patient surveys where patients are providing feedback that they are feeling supported and ready to go home” from the hospital.
The solutions we are developing are spreading to every organization across the Osakidetza-Basque Health Service.
Looking overseas for examples of widespread impact, Osakidetza-Basque Health Service in Spain, which runs the public health-care system in the Basque Country, had inspiring outcomes to share with its Ibero-American counterparts at a recent gathering. This Host coordinates the BPSO centres within the region, which provides primary care, mental health, acute care and long-term care to a population of 2.2 million people across 17 health organizations.
“The solutions we are developing within the system are spreading to every organization across the Osakidetza-Basque Health Service. If we create a new (BPG-derived) protocol or have something that needs to be implemented, it’s not just done in the BPSO-affiliated organizations, but throughout the entire region. This has a ripple effect,” says Maria Angeles Cidoncha-Moreno, head of teaching and research in nursing. According to BPSO co-lead Lucía Gárate Echeñique, coordinator of strategy and nursing projects, the implementation of BPGs – focused on least restraints, breastfeeding, falls prevention, pressure ulcer prevention and vascular access – has been impactful.
For example, by implementing the Promoting Safety: Alternative Approaches to the Use of Restraints BPG at Bizkaia Mental Health Network (one of the region’s BPSOs), Cidoncha-Moreno and Gárate Echeñique expanded the work on verbal de-escalation and patient comfort plans to help patients feel calmer across the system.
“Everything aligned, and a multidisciplinary working group was created to represent not only the original mental health centre but all stakeholders. This led to the development of a policy at the public health system level, with a protocol that maximizes the impact of what was initially implemented at the (mental health) centre,” says Gárate Echeñique.
This BPG – and others – is also being disseminated across Basque province through webinars and peer-to-peer, which is changing the way providers care for patients. By 2024, physical restraint use across the Osakidetza-Basque Health Service was cut by more than half.
Impact on a new generation of nurses
The positive impact of BPGs can also be seen in the way nursing students are educated.
Thunder Bay’s Confederation College Practical Nursing Program is working to become the first academic BPSO to implement the Transitions in Care and Services BPG into its curriculum. BPSO co-leads Jamis Robins and Dr. Michael Scarcello have changed language in course outlines and assignments and added more knowledge, skills and course learning outcomes that are in line with recommendations in the BPG.
The college is a partner in the Indigenous BPSO program, and as such must ensure the implementation of the BPG honours Indigenous ways of knowing and supports holistic community wellness. “We…looked at where (the BPG) makes sense (to implement) and where does it fit,” says Robins. “(We’re) taking the art of nursing and trying to balance it with evidence…(while) really looking at the cultural aspects of Indigenizing our content.” They also work with Oshki Wenjack, a post-secondary training institution founded by the 49 Indigenous communities of the Nishnawbe Aski Nation to offer support and strengthen culturally enriched learning.
Scarcello is asking students to be more culturally aware when working on lab assignments. “We’re encouraging them to use things like art to provide patient education…(and) land-based activities,” he says. The goal is to not “…follow the status quo, but to actually ask people what is it that you need as an Indigenous person going back to your community?”
Confederation College is only in the first year of its BPSO journey, and Scarcello says he’s already seeing students step up as leaders in evidence-based care. “They have the information at their fingertips. They don’t have to go look for (BPGs)…and we’re teaching them how to use it and not to be afraid of evidence,” he says. Over time, he expects to see an impact on patients, families and communities across northern Ontario.
Internationally, Portugal’s Escola Superior de Enfermagem do Porto (ESEP), which joined as an academic BPSO in September 2024, is preparing for the impact BPGs will have on its students.
“We are excited about the potential impact (these BPGs) will have on the education of our students and the quality of health care in Portugal. We believe the implementation of BPGs will transform how we prepare our students for the challenge of clinical practice, enhancing client safety, satisfaction and the continuous development of future nursing professionals,” says Marisa Lourenço, adjunct professor and BPSO lead.
Four other academic institutions in Portugal have since joined the program, she adds, and all will be implementing BPGs into their nursing curriculum, including Person- and Family-Centred Care, Practice Education in Nursing, and Assessment and Interventions for Perinatal Depression.
BPG implementation is constantly evolving and with it so do the ways we measure and evaluate its impact, Naik says. Through quantitative (data) and qualitative (anecdotal) methods, organizations measure their health outcomes at the individual, organizational and health system levels. This is critical from an organizational perspective, and also from an RNAO perspective in terms of the purposeful evolution of the BPG program. “It’s important we always evaluate impact and showcase the value of evidence-based practice on outcomes, and use that evidence to continue to grow as a program.”