As we mark 25 years of RNAO’s Best Practice Guideline (BPG) Program, we would be remiss if we did not take a closer look at how today’s social landscape informs BPGs and the work of Best Practice Spotlight Organizations® (BPSO®). The issues of anti-Black racism, Indigenous health, 2SLGBTQI+ health equity and harm reduction are social concerns that RNAO addresses.
So, what do these social issues have to do with BPGs?
Simply put: Lots.
RNAO’s relentless commitment to evidence-based healthy public policy and equity BPGs serves to inform nursing practice in clinical settings, academic institutions, research, policy and administration.
Let’s take a closer look at these social issues in the context of the BPGs that inform nursing practice in these areas, and the ongoing and crucial advocacy of BPG champions, BPSO leads and RNAO to stay true to a commitment that places patients, clients and community members at the core of practice change and policy development.
ANTI-BLACK RACISM IN NURSING
Work began in October 2023 on a new RNAO BPG focused on anti-Black racism in nursing, set for release in February 2026. Leading this work are RNs and co-chairs Dr. Bukola Salami, Canada Research Chair in Black and Racialized Peoples’ Health, and Dr. LaRon Nelson, Associate Dean for Global Health & Equity and Independence Foundation Associate Professor of Nursing at Yale University.
“We know that anti-Black racism is real,” Salami explains. “Black people experience disparities, and Black nurses…have challenges in terms of access to leadership and…face micro-aggressions.” Despite this, she says the social landscape has shifted since the early days of the racial reckoning tied to the murder of George Floyd in 2020. “What we’ve seen lately is a rise against...EDI (equity, diversity and inclusion) initiatives,” Salami says. “And we have to keep asking ourselves: How can we strategize and continue to address issues related to inequities and disparity?”
“I think this BPG…will be very well-positioned to continue the momentum and provide tools that people can use to address anti-Black racism,” Salami predicts. Shutting out the noise and focusing on recommendations that draw on the experiences of the panel is foremost in her mind as co-chair.
“We all bring in our lived experience in the clinical setting...in the educational setting.... We are drawing from lived experience and also educational experience to inform the BPG…to ensure it is of benefit and of impact to nurses and ultimately to patient care.”
Nadia Prendergast, an RNAO Recognition Award winner and a member of the expert panel, wrote a book on the subject – An introduction to anti-racism for the nursing professional – in 2023. The Toronto Metropolitan University faculty member says there’s still a “quietness” around anti-Black racism despite it being a “critical social issue.” But that won’t deter strong advocates like those on the BPG panel.
It isn’t just going to help Black nurses; it’s going to help white nurses and racialized nurses too. We’ll have a competency that’s diverse rather than a competency that looks from one lens.
“What we’re seeing now is more research, more studies, more Black professors and Black scholars who have a space to talk,” she suggests, adding “…there are social and health determinants that show anti-Black racism is prevalent in our health systems, our education systems…in all systems.” Nurses “…need to be more active in being critical allies and being an agency that speaks against anti-Black racism. We have a responsibility to make change, and we can’t do it separately, we have to do it together.”
The BPG is a tool to help us and it’s for all nurses, Prendergast says.
“It isn’t just going to help Black nurses; it’s going to help white nurses and racialized nurses too. We’ll have a competency that’s diverse rather than a competency that looks from one lens. Even though we’re doing work that has to do with equity, sometimes we build our own enclaves and get stuck in that. Let’s open these doors so we can walk into each other’s understanding.”
Prendergast says she “gets a lot” from her work on the panel. “With change, there’s going to be pain and discomfort, and I can walk with (colleagues) through this discomfort. I can walk through my own discomfort and my own pain. But the process of walking through this pain will transform me into a better person and will transform my colleagues to be better.”
Salami says the panel is a strong group of Black nurses who are committed to social justice and equity. And there’s an acknowledgement that the work isn’t done when the BPG is published. “Even after the BPG, we must continue on the journey towards equity. It’s not about reaching a goal (the BPG) and we’re done. It’s a continuous process.”
Pairing practice change with broader RNAO advocacy
RNAO’s Black Nurses Task Force (BNTF) was launched in June 2020 following brutal acts of anti-Black racism and discrimination in Canada, the U.S. and around the world. The murder of George Floyd at the hands of law enforcement was an atrocity that led to a movement of solidarity to stop inequities based on the colour of one’s skin.
The mandate for BNTF is to reduce anti-Black racism and discrimination within the nursing profession. It released its Task Force report with 19 recommendations in February 2022. The formation of RNAO’s Black Nurses Leading Change (BNLC) interest group was inspired by the task force recommendations. This group advocates for mentorship, educational supports and networking opportunities for Black nurses.
For resources and information about this ongoing work, plus examples of members making a difference, visit the Black nurses and RNAO In Focus website.
INDIGENOUS HEALTH
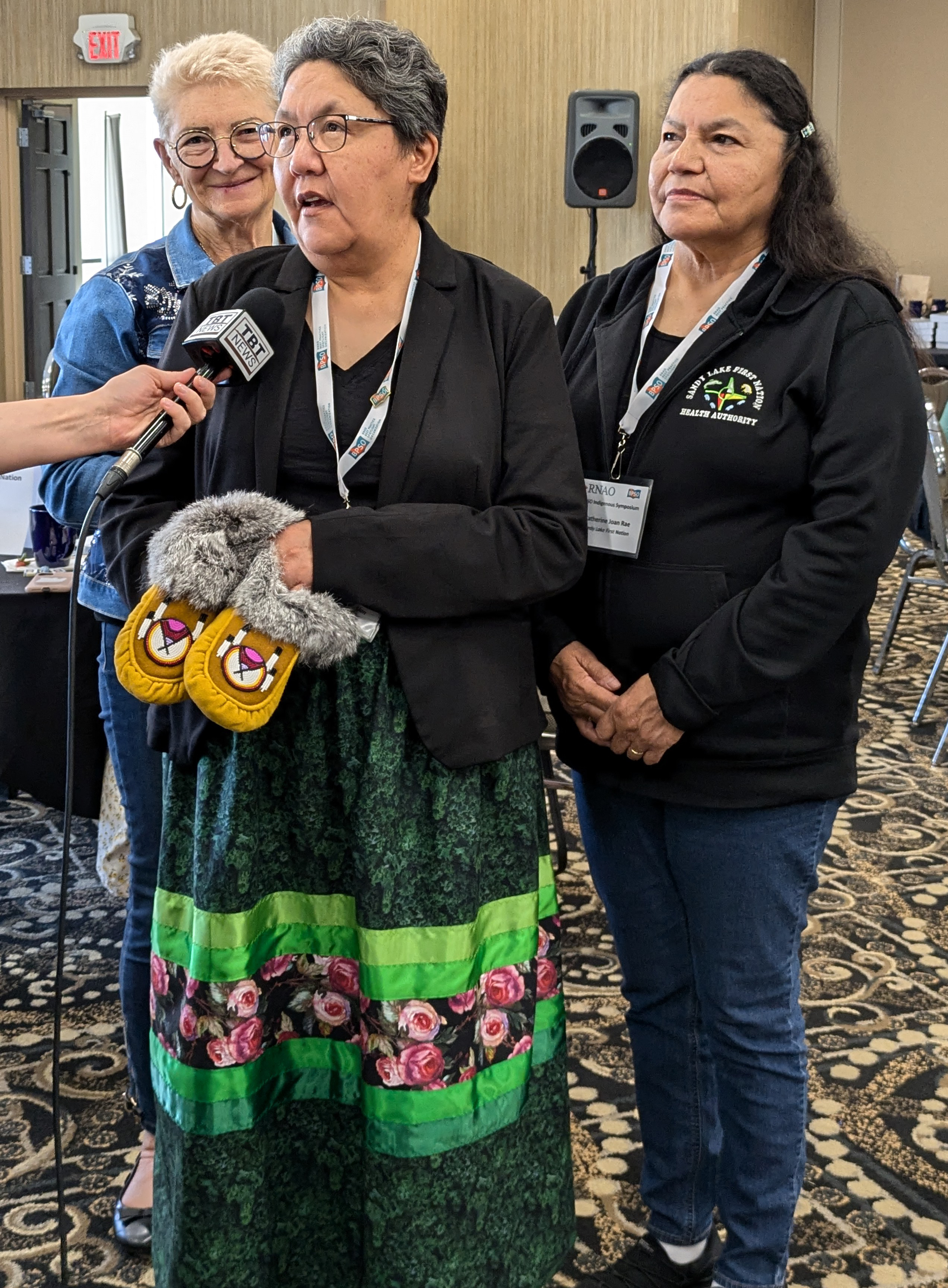
In 2022, RNAO’s first Indigenous-focused BPG was published: Promoting Smoking Reduction and Cessation with Indigenous Peoples of Reproductive Age and Their Communities. A second guideline focusing on life promotion and youth suicide prevention is being developed.
Greta Meekis is a child wellness coordinator and the BPSO lead for Sandy Lake First Nation, located 600 kilometres northwest of Thunder Bay. She and her team wanted to implement the BPG because of its suggestion that wholistic health assessments should include conversations about smoking, in a culturally safe way.
Meekis, who is Indigenous, has played a critical role in her community and in RNAO’s Indigenous-focused programs. “Her leadership and authenticity are contagious,” says RNAO CEO Dr. Doris Grinspun, founder of the BPG program. Drawing on her invaluable personal and community perspective, Meekis is now serving as co-chair for the suicide prevention BPG.
If we can change one person’s opinion or perspective, that has a big impact...and that’s the start of the change.
“We lost a champion a year ago due to suicide. She was part of the team, and helped the team move forward and grow,” Meekis remembers fondly. The trauma of that loss has stirred a need in Meekis to participate in the new BPG. “For my healing journey, I feel I need to try and help others. We’ve lived it, and we as a team at Sandy Lake…recognize the gaps. There’s the before, during and after (with suicide). There’s a lot of prevention and a lot of support during, but the after…there’s a lot of gaps…there’s something lacking there. As part of the panel for the new BPG, we can be part of the change and bring more awareness to this.”
BPG implementation for Sandy Lake – which is also implementing guidelines on peri-natal depression and person- and family-centred care – is all about one-on-one communication with clients, Meekis explains. “If we can change one person’s opinion or perspective, that has a big impact for us because that one person will let others know, and that’s the start of the change.”
One of the team’s most successful awareness building campaigns came in the form of a radio show in the spring of 2023. Everyone in the community loves to tune in to the local station, and many listeners are engaged by calling in to win prizes, Meekis says.
To raise awareness of the dangers of smoking, the health unit hosted a special guest on the show to discuss the evidence about smoking, and to raise the issue that tobacco used in cigarettes contains sugar. Considering a lot of people in the community have diabetes, there was a lot of reaction to this, Meekis recalls. With prizes to hand out for the correct answers in a follow-up, call-in quiz, Meekis was happy with the engagement of the community.
“I can’t tell people they can’t smoke in their own homes,” she says. But sharing the evidence in the BPG and suggesting they consider that evidence when they’re deciding whether to smoke around their child – that’s the approach she feels works well in Sandy Lake. “We say don’t hold your baby for 20 minutes after smoking because the carbon monoxide will linger – this is what the evidence shows us.” And educating the community and raising awareness of the evidence is her primary goal.
“I feel we do make a difference,” Meekis says hopefully. “There’s no right or wrong way to accomplish what we want to accomplish. Even one individual at a time.” One step at a time is the goal for Meekis and her team. “Having an impact makes you smile and try even more the next day,” she says.
Pairing practice change with broader RNAO advocacy
A decade ago (2015), Canada’s Truth and Reconciliation Commission issued 94 calls to action aimed at addressing the legacy of residential schools and advancing reconciliation. Seven of those calls were focused specifically on health (numbers 18-24). Nurses are actively contributing in many ways to improved Indigenous health and the fulfilling of these calls to action. RNAO’s Indigenous Nurses and Allies Interest Group (INAIG) was formed in 2021 to mobilize nurses and raise awareness of the impact of ongoing systemic racism, discrimination and inequities in the nursing profession and health system that impact Indigenous health and wellness.
In 2018, RNAO secured government funding to partner with key Indigenous groups to address the health and social inequalities that Indigenous communities continue to face. By March 2019, eight Indigenous communities formally signed BPSO partnerships with RNAO and all are thriving. More have joined since and more are planning to sign in 2025.
For resources and information about this ongoing work, plus examples of members making a difference, visit the Indigenous health and RNAO In Focus website.
2SLGBTQI+ HEALTH EQUITY
Advocacy by and for the 2SLGBTQI+ community has been a priority for RNAO for the last two decades. The association partnered with experts, allied health professionals and people with lived experience to create the Promoting 2SLGBTQI+ Health Equity BPG in 2021. Quest Community Health Centre in Niagara Region is one of 10 BPSOs currently implementing the guideline.
“We were really excited when this particular BPG became available,” says Jenny Stranges, Quest’s program director. Implementation “…was a good opportunity to examine the work we’d been doing and think about how we could further grow it…in a way that aligns with data and clinical best practices.”
The 2SLGBTQI+ population represents about 40 to 45 per cent of clients visiting Quest, which is the third-largest trans clinic in Canada (the others are in Toronto and Vancouver). These individuals are from Niagara Region primarily, but also travel from other communities such as Oakville, Burlington and Hamilton. And they’re travelling because they’ve heard good things about Quest.
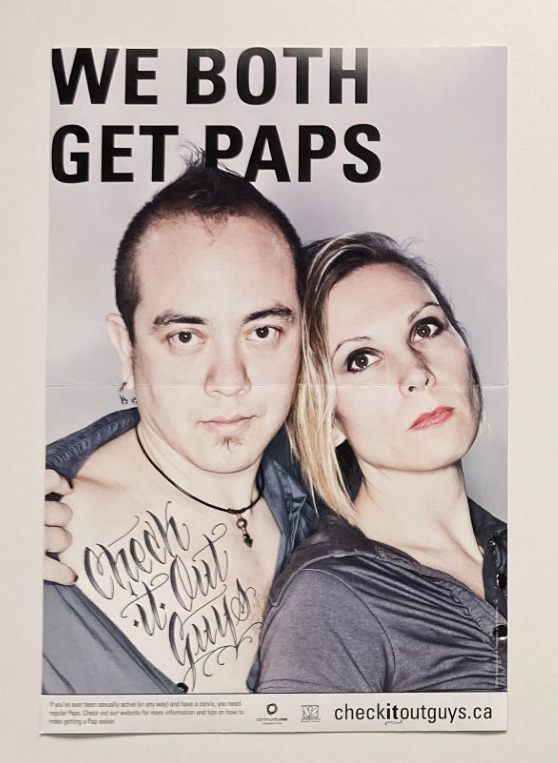
One service that has garnered positive attention is cervical cancer screening through Papanicolaou (PAP) tests.
“PAPs are not something people enjoy,” says Quest RN Kim Parise. After the test, clients receive an anonymous survey “…and what’s happening is people are telling their friends this is a really safe and positive environment to come and get your (test).” Parise says comments on the surveys have ranged from “this is a safe space” to “people are very respectful” to “this is as professional as I’ve ever seen” and “it was very simple.” And she notes she’s seeing more people coming in for tests.
Any medical procedure is incredibly anxiety-provoking because you’re never quite sure how you’re going to be perceived.
“For individuals who are non-binary or who identify as trans…any medical procedure is incredibly anxiety-provoking because you’re never quite sure how you’re going to be perceived,” Stranges adds. “It’s always an uphill battle around ensuring that your preferred pronouns are being used, and people understand your preferences around language, around body parts…and just respecting your dignity.”
Quest’s general client experience survey, handed out by providers after appointments or to clients in the waiting area, has also resulted in positive feedback. According to Ailish Westaway, a health promoter and the BPSO lead at Quest, 100 per cent of 2SLGBTQI+ clients who completed the survey in 2023 responded that Quest uses language that makes them feel included, and 92 per cent felt Quest welcomed them and treated them in a non-judgmental way.
“Interactions with the health-care system have been unfortunately historically quite painful for the population,” Stranges says. “Building that trust and word-of-mouth that it is a place you can come, feel safe, feel respected and have boundaries respected – it makes a big difference.”
As a BPSO, Quest is implementing a total of eight RNAO BPGs. It participates on several community committees and works with community partners such as Rainbow Health Ontario to raise awareness at events and conferences. It works with other community care partners to train-the-trainer on culturally competent care for the 2SLGBTQI+ community accessing post-operative services, which can be challenging after gender affirming surgery. Quest also works closely with Niagara Region’s Ontario Health Team to ensure the needs of the 2SLGBTQI+ population are represented in all health sectors.
“The BPG is so important because…(2SLGBTQI+ health equity) is an ever-changing and evolving (issue). It takes work. You have to keep working at it and this is a great opportunity to keep working and evolving as an organization.”
Read more about the impetus for the BPG, and the lived experiences of some of its panel members in the Winter 2022 issue of RNJ.
Pairing practice change with broader RNAO advocacy
RNAO has called on the provincial government to commit to creating safe spaces for the 2SLGBTQI+ community. RNAO has also repeatedly called on the leader of the federal opposition – Pierre Poilievre – to stop targeting transgender and gender-diverse youth.
The association’s Rainbow Nursing Interest Group (RNIG) was formed in 2007, and members have proudly held the RNAO banner at every Pride Parade since. Members have also brought resolutions to the AGM calling on governments and health leaders to include the health needs of sexual and gender minorities in nursing curriculum. RNAO’s position statement on Respecting Sexually and Gender Diverse Communities was published in 2021, developed in partnership with the RNIG.
Physical and mental health inequities are often experienced differently by 2SLGBTQI+ people. Their health outcomes are impacted by the intersection of gender identity, gender expression and sexual orientation with other determinants of health such as age, income, disabilities, ethnicity or race.
For resources and information about this ongoing work, plus examples of members making a difference, visit the 2SLGBTQI+ and RNAO In Focus website.
HARM REDUCTION
RNAO has published three BPGs that offer recommendations for optimal care through a harm reduction lens. The first (now retired) focused on supporting clients on methadone maintenance and treatment (2009). The second and widely implemented BPG is focused on Engaging Clients Who Use Substances (2015). A third BPG, released in 2018, provides recommendations for Implementing Supervised Injection Services.
Thunder Bay Regional Health Sciences Centre (TBRHSC) is one of the BPSOs implementing the 2015 guideline.
RN Giulia Daniele is its addictions medicine and mental health clinical nurse specialist and best practice champion. She assumed her role in June 2023, when TBRHSC acknowledged the need for an individual dedicated to this work. Thunder Bay has been identified as the number-one city for opioid overdose deaths per 100,000, she explains. “That was a major contributor to us doing some of this work because we recognized there was a concern.”
In her role, Daniele supports staff who have questions and concerns in relation to mental health and substance use. She leads efforts to educate colleagues on stigma, harm reduction and trauma-informed care, and improves policies and procedures to support nurses who work with patients who use substances. The BPG “helps guide a lot of our initiatives…any time policies and procedures come about…we are looking to see what is in the BPG and how we can implement that into our practices.”
Daniele works closely with RN Kim Gross, who was also hired to raise attention to harm reduction in acute care. On a referral basis, Gross assesses patients and supports their families in collaboration with the health-care team and ensures seamless discharge to the community by connecting with external partners. This transition is critical to ensure patients and families continue to get what they need, when and where they need it.
In fact, it became even more critical in August 2024, when Path 525 – a supervised consumption services (SCS) site operated by the NorWest Community Health Centre in Thunder Bay – received notice that it would be one of 10 Ontario sites closing in March 2025 (read more below and in RNAO’s response to the news of the closures).
Tali Magboo Cahill is an Ottawa acute care RN and the former eastern Canada representative for the Harm Reduction Nurses Association of Canada. She helped plan and acted as a panelist in a webinar hosted by RNAO’s Mental Health and Substance Use Program.
The webinar focused on the need for increased harm reduction efforts in hospital settings. Nurses in acute care are uniquely positioned to help people who use substances, she says. “We have the ability to make or break a patient’s day and to work with them on making them comfortable. I think that’s a power we need to recognize…when people are in a very vulnerable time.”
“Harm reduction is evidence-based practice for people who use drugs. There’s a growing gap between what’s happening in the community…and what’s happening in the hospital. The more this gap grows…the poorer we’re serving our patients,” she says.
Acute care nurses are often unsure of their harm reduction role(s) because there are limited policies and procedures that clearly define what they should be doing, Magboo Cahill adds. But “...you don’t need a policy to give you permission to treat people with empathy and to treat them well,” she reminds nurses. “You don’t need a policy to be non-judgmental.”
Pairing practice change with broader RNAO advocacy
Since the Ontario government’s August 2024 announcement to close SCS sites, RNAO has been forcefully stating that the decision will lead to unsafe communities, increased deaths, overwhelmed emergency services and escalating health-care costs. “Our health system treats those with cancer and chronic illnesses with compassion and with comprehensive services,” RNAO CEO Dr. Doris Grinspun has said repeatedly. “We must extend the same care to persons dealing with substance use.” RNAO is calling for the government to adopt an integrated care model that supports both harm reduction and treatment services.
RNAO members have also been vocal, joining other concerned allies at rallies and protests. They have met with decision makers in their own communities to discuss concerns and provide a frontline view on the issue. Drawing on lived experiences and the power of the evidence, members are raising awareness that the defunding of harm reduction programming places ideology over health care.
For resources and information about this ongoing work, plus examples of members making a difference, visit the Substance use, mental health and RNAO In Focus website.
Health Equity Consortium
RNAO’s Health Equity Consortium brings together three interest groups – Black Nurses Leading Change, Indigenous Nurses and Allies Interest Group and Rainbow Nursing Interest Group – to work alongside the Black Nurses Task Force, RNAO's CEO, and many other key staff to share perspectives and experiences, identify collective actions to power all members to end racism and all forms of discrimination, enrich nurses’ careers, and improve health care for all.
For resources and information about the Health Equity Consortium, visit the RNAO and Health Equity In Focus website.